Some questions arrive quietly, almost the way an unsettled night lingers without explanation.
“Can I have sleep apnea if I don’t snore?” is one of those thoughts that slips in when mornings feel heavier than they should or when rest never seems to refresh the way it once did.
Silence can be comforting, but it can also blur the signals the body tries to send.
Not every experience shows itself through sound; sometimes it’s the absence of it that invites deeper attention.
As you move through these lines, let yourself pause, listen inward, and consider what your quiet nights may be trying to express.
What Is Sleep Apnea? A Simple Explanation
Sleep apnea is a condition in which breathing slips in and out during sleep, creating small pauses that interrupt the natural rhythm of the night.
These pauses can last several seconds and recur repeatedly, often without leaving any lasting memory.
The body gently pulls you from deeper rest each time, just enough to start breathing again, but never enough to feel fully awake.
Over time, these constant interruptions soften the quality of sleep, leaving the mind and body without the deep restoration they’re reaching for. What seems like a full night can turn out to be far less replenishing.
The Big Myth: “No Snoring Means No Sleep Apnea”
Many people assume sleep apnea always announces itself with loud snoring, yet it can go unnoticed in its silence.
This belief often keeps real signs unnoticed. Persistent exhaustion, morning heaviness, or quiet moments of gasping observed by a partner can all hint at deeper disruptions, even when the night seems soundless.
Understanding the Three Types of Sleep Apnea
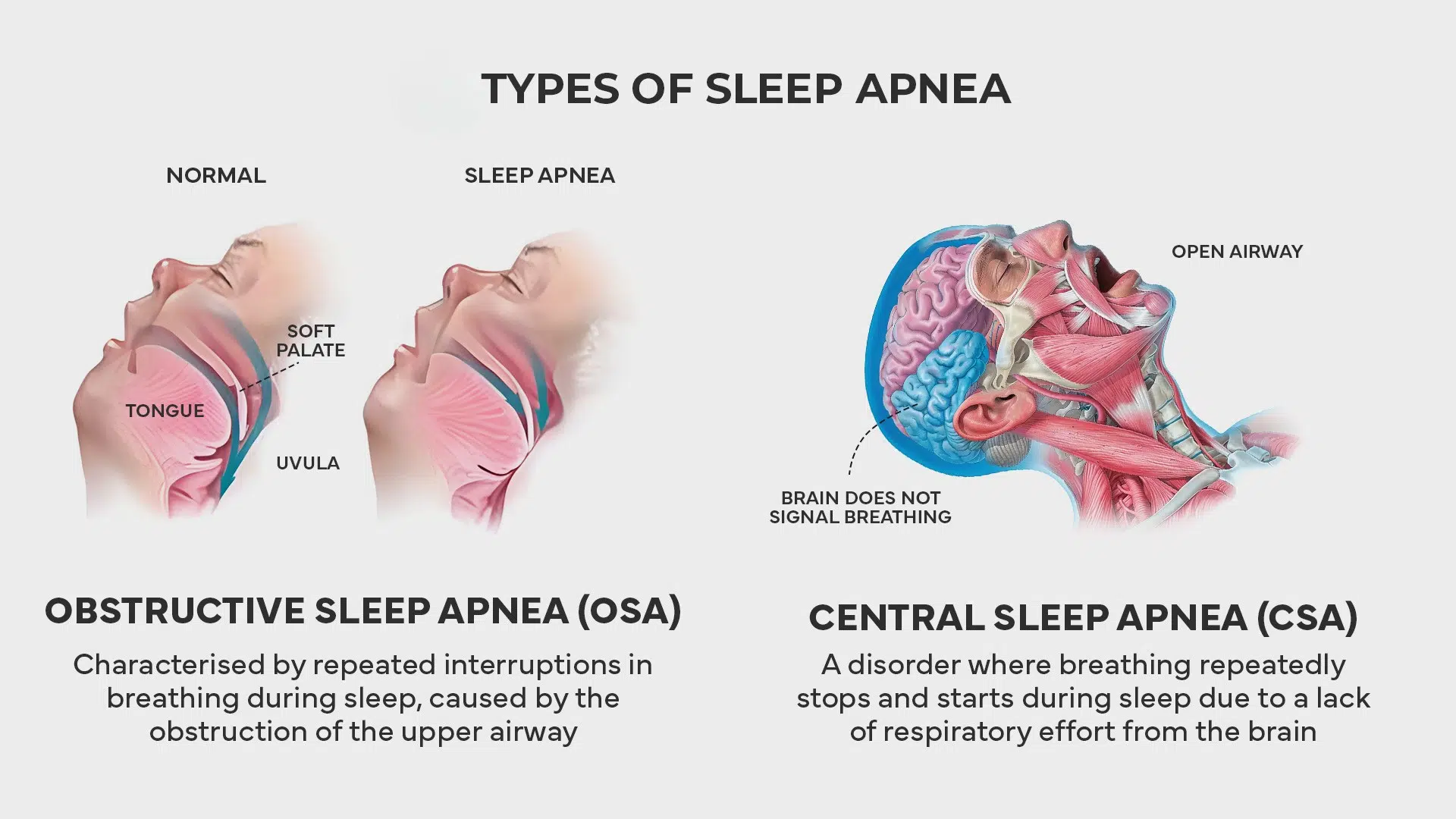
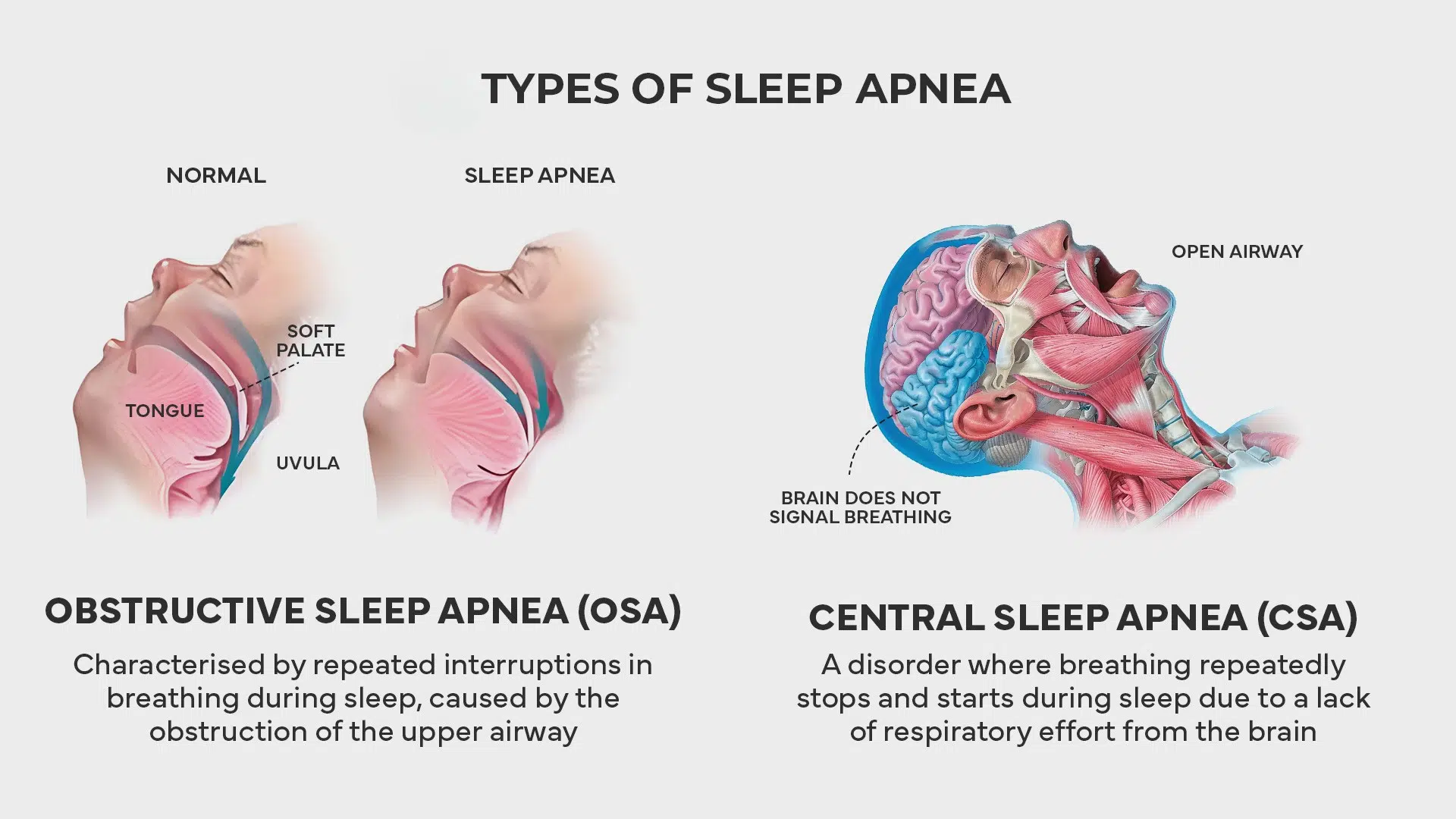
Not all sleep apnea is the same. There are three main types, and each affects your breathing differently:
1. Obstructive Sleep Apnea (OSA)
This is the most common type, affecting about 90% of people with sleep apnea. OSA occurs when the muscles in your throat relax during sleep, narrowing or completely closing your airway.
Does it cause snoring? Often, yes, though not always. Some experience quiet obstruction, where airflow shifts without creating the familiar vibration of sound.
2. Central Sleep Apnea (CSA)
This type is much less common, accounting for about 10% of cases. With CSA, your brain fails to send the proper signals to the muscles that control breathing. Your body simply doesn’t try to breathe for short periods.
Does it cause snoring? No. Since there’s no physical blockage or breathing effort, central sleep apnea typically doesn’t produce snoring. This makes it even harder to detect.
3. Complex Sleep Apnea Syndrome (CompSAS)
Also called treatment-emergent central sleep apnea, this condition is a combination of both obstructive and central sleep apnea. Some people develop it after starting CPAP treatment for OSA.
Does it cause snoring? Sometimes. Sound varies as patterns shift between obstruction and pauses, creating nights that move between quiet moments and subtle changes in airflow.
Why Sleep Apnea Can Occur Without Snoring
Sometimes the body moves through the night in quiet patterns, offering no sound, yet carrying subtle interruptions that reshape how rest unfolds.
- Brain-based breathing patterns: Central apnea pauses breathing without obstruction, creating silent nights where the body’s rhythm shifts quietly beneath the surface.
- Mild airway collapse: Gentle narrowing softens airflow, disrupting sleep without producing the familiar vibration that usually turns breaths into sound.
- Individual anatomy: Unique airway shapes influence vibration, allowing disturbances to pass quietly even when breathing patterns drift away from ease.
- Sleep position: Side-sleeping lessens vibration, yet breathing pauses can still appear softly, hidden within the stillness of the night.
Silence can feel comforting, yet it doesn’t always mean ease; sometimes it reflects quiet disruptions, inviting a deeper look at rest.
Why Silent Sleep Apnea Is So Dangerous


Silent sleep apnea moves quietly through the night, leaving few clues, yet its hidden disruptions can deeply influence the heart, mind, and overall well-being.
1. Cardiovascular Risks
Silent apnea repeatedly lowers oxygen levels, prompting stress responses that strain the heart.
Over time, these quiet interruptions contribute to high blood pressure, rhythm disturbances, and increased chances of heart disease or stroke, even when nights appear peaceful.
2. Metabolic Consequences
Disrupted sleep affects hormone balance, appetite, and blood sugar control.
These subtle changes can encourage weight gain, heighten diabetes risk, and weaken the body’s ability to manage insulin, making silent apnea a significant contributor to long-term metabolic strain.
3. Cognitive and Mental Health Effects
Interrupted breathing fragments deep rest, affecting the brain’s ability to process information and regulate emotions.
This can lead to forgetfulness, slower thinking, heightened irritability, and lingering feelings of anxiety or sadness that shift how daily life is experienced.
4. Safety and Quality of Life
Daytime fatigue from restless nights affects attention, mood, and relationships.
It raises accident risk, reduces work performance, and creates emotional distance, gradually shaping life in ways that feel heavier and less connected than they should.
The Hidden Warning Signs
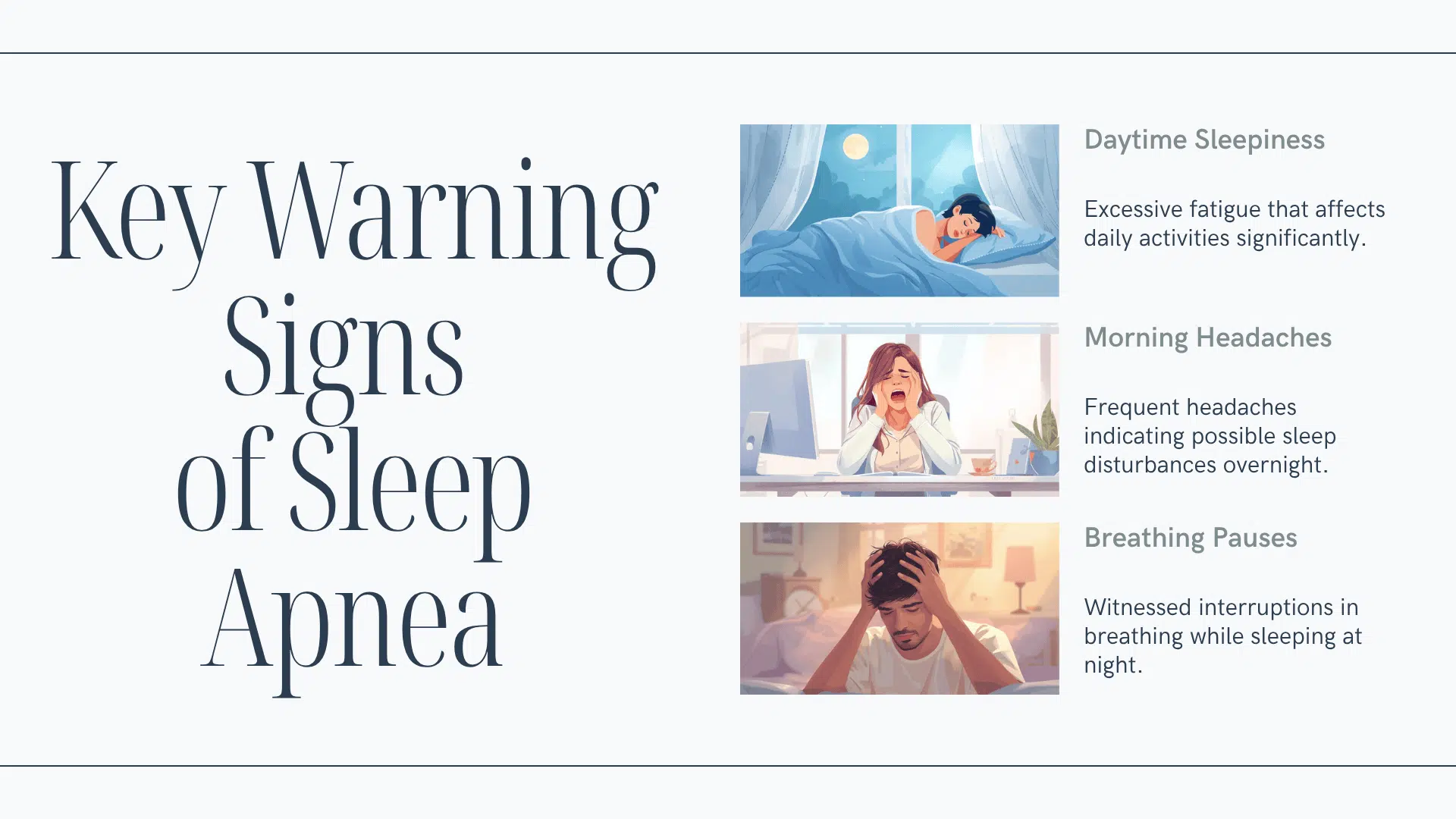
When nights remain quiet, the body often communicates through softer signals, offering gentle reminders that rest may not be unfolding naturally.
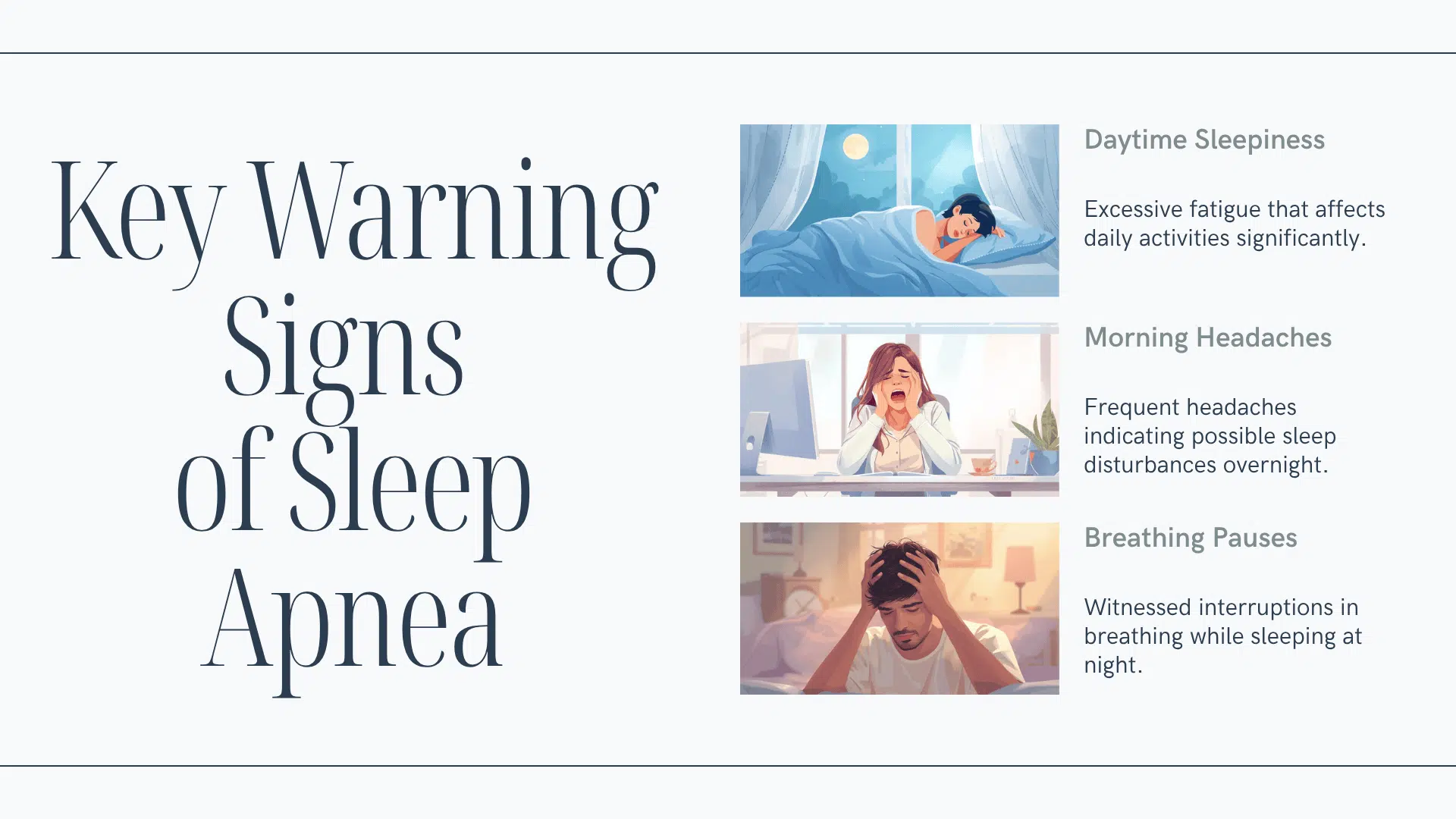
Daytime Symptoms
- Extreme tiredness: Persistent exhaustion lingers through the day, even after seemingly adequate hours of sleep.
- Morning headaches: A heavy, squeezing discomfort greets you on waking, lingering longer than you expect.
- Difficulty concentrating: Focus drifts easily, leading to memory lapses and mental fog during daily tasks.
- Mood changes: Unexpected irritability or sadness rise without a clear cause, coloring simple moments.
- Falling asleep easily: Sudden drowsiness appears during still activities, quietly reshaping everyday safety and presence.
Nighttime Symptoms
- Waking up gasping: Sudden breaths pull you awake, breaking the stillness of the night unexpectedly.
- Frequent awakenings: Sleep fragments into brief moments, leaving the night feeling disjointed and shallow.
- Dry mouth or throat: Mornings bring a parched sensation, hinting at disrupted night breathing.
- Increased urination: Repeated nighttime bathroom visits subtly interrupt your natural sleep rhythm.
- Restless sleep: Sheets tangle easily as the body shifts repeatedly in search of comfort.
What Others May Notice: Pauses in breathing, shallow or irregular breaths, small body jerks, or quiet gasping sounds during sleep.
Who’s at Higher Risk?
Some patterns make silent sleep apnea more likely, creating a quiet vulnerability that unfolds slowly, shaped by age, lifestyle, and underlying health.
| Risk Factor | Why It Matters |
|---|---|
| Age | Risk rises naturally with time, especially beyond forty. |
| Sex | Men face higher rates; women’s risk increases significantly after menopause. |
| Weight | Extra weight around the neck gently narrows the airway during sleep. |
| Neck circumference | Larger measurements suggest reduced airway space, raising the likelihood of breathing interruptions. |
| Family history | Genetic patterns can quietly influence airway shape or breathing control. |
| Medical conditions | Heart failure, stroke, or high-altitude exposure can affect nighttime breathing stability. |
| Medications | Long-term opioid use may disrupt the brain’s breathing signals during sleep. |
Understanding these patterns offers a quiet clarity, helping you notice when subtle risks may be shaping how your nights unfold.
Begin the Diagnostic Process


Some moments call for gentle attention, especially when quiet signs begin to shape your nights and nudge you toward deeper clarity about your sleep.
Step 1: Speak With Your Doctor
Share your symptoms, sleep patterns, medications, and family history openly.
This simple conversation creates a clearer picture of your concerns and helps your doctor understand the subtle shifts affecting your rest.
Step 2: Find Sleep Study Options
An in-lab sleep study offers the most detailed insight, gently tracking brain activity, breathing, oxygen levels, and movement through the night.
A home sleep apnea test provides a simpler option for many, using portable equipment to record breathing and oxygen changes while you sleep in your own space.
Step 3: Understand Your Results
Your report includes anApnea-Hypopnea Index (AHI) showing how often breathing pauses occur each hour:
- Normal: fewer than 5
- Mild: 5–14
- Moderate: 15–29
- Severe: 30 or more
These numbers help clarify the depth of your sleep disruptions and shape the next steps in your care.
Treatment Options That Work
Finding the right support begins gently, with treatments that steady your breathing, soften your nights, and guide your body toward deeper, calmer rest.
-
CPAP therapy: Delivers a gentle stream of air that keeps your airway open, helping your body settle into deeper, uninterrupted, restorative sleep.
-
Oral appliances: Deliver subtle jaw or tongue repositioning, encouraging smoother airflow and offering a quieter, more comfortable approach for milder sleep apnea experiences.
-
Adaptive servo-ventilation (ASV): Delivers real-time airflow adjustments that guide your breathing into steadier patterns, especially helpful for central or complex sleep apnea.
-
Lifestyle changes: Deliver small, meaningful shifts, like side sleeping, weight balance, or reduced alcohol, that quietly support easier breathing and calmer nightly rhythms.
-
Surgical options: Deliver structural improvements that open blocked pathways when other treatments fall short, making breathing smoother and more consistent through the night.
-
Treating underlying conditions: Delivers stability by addressing heart issues, medication effects, or altitude changes, gently reducing the disturbances behind central sleep apnea.
Each option offers its own quiet form of support, helping your nights grow steadier and guiding your body toward breathing with greater ease.
What Sleep Doctors Want You to Know
|
Prevention and Long-Term Management
Healing begins with small, steady choices. Once treatment starts, consistency becomes the quiet thread that helps your nights grow calmer and your days feel lighter.
- Use your therapy every night: CPAP or oral devices work best when woven into your nightly rhythm without interruption.
- Follow up with your doctor: Regular visits offer time to adjust, refine, and ensure your treatment continues to support you.
- Monitor your symptoms: Notice how your body feels and share any shifts that appear along the way.
- Maintain healthy habits: Gentle lifestyle changes continue nurturing your progress long after treatment begins.
- Replace equipment when needed: Masks and supplies soften with time, and refreshing them keeps your therapy comfortable and effective.
Staying attentive to your routines creates a quiet foundation for long-term ease, allowing each night to restore you more fully than before.
The Bottom Line
Silent sleep apnea is real, dangerous, and more common than many people realize. The absence of snoring can actually make the condition harder to detect, leading to delayed diagnosis and treatment.
If you recognize any of the symptoms described in this article, extreme daytime tiredness, morning headaches, difficulty concentrating, or witnessed breathing pauses, don’t wait.
Talk to your doctor about a sleep study. Early diagnosis and treatment can protect your heart health, improve your quality of life, and may even save your life.
Remember: sleep apnea is a serious medical condition, but it’s also highly treatable. Taking that first step toward diagnosis could be the best decision you make for your health.
Frequently Asked Questions
Can Silent Sleep Apnea Affect Dream Quality?
It can gently disrupt deeper sleep stages, making dreams feel faint, fragmented, or harder to remember.
Does Silent Sleep Apnea Change Morning Mood?
Subtle nighttime interruptions may create softened energy, shaping your morning mood with unexpected heaviness or irritability.
Can Silent Sleep Apnea Worsen During Travel?
Changes in routine, altitude, or sleep position can quietly intensify nighttime breathing disruptions while away.
Does Drinking Water Before Bed Persuade Silent Apnea?
Hydration itself doesn’t cause events, but nighttime awakenings may feel more frequent when bladder interruptions occur.