Snoring so loud you wake up the neighbors? Partner threatening to sleep in the garage? Welcome to the CPAP club nobody wants to join.
You probably already know you need one of those breathing machines. But then someone drops the bomb: “First, you need a sleep study.” Ugh. Really?
Picture this: waiting three months for an appointment. Driving to a medical building at 8 PM. Trying to fall asleep while a technician watches you through a window.
Sounds fun, right? Not really.
Here’s what they don’t tell you. You might not need all that drama. There are actually several ways to get CPAP therapy without the traditional sleep lab routine.
Some are faster. Some are way cheaper. And all of them can help you stop feeling like a zombie every morning. Let’s talk about your real options.
Understanding CPAP and the Role of Sleep Studies
Think of a CPAP machine as your personal breathing buddy.
CPAP stands for Continuous Positive Airway Pressure. It pushes gentle air through a mask while you sleep. This keeps your airway open.
Here’s the problem: Your throat muscles relax during sleep. They collapse and block your airway. You stop breathing. Your brain panics and wakes you up. Research shows this happens up to 400 times per night in severe cases.
CPAP fixes this by delivering steady air pressure. It props your airway open like a gentle air splint. No more breathing pauses. No more constant wake-ups.
Better sleep means more energy and clearer thinking.
Why Sleep Studies Are the Gold Standard
Sleep studies are incredibly thorough. They track everything – brain waves, breathing patterns, oxygen levels, and heart rhythm.
Two main types exist:
Lab Sleep Study – Full overnight monitoring in a medical facility. Most comprehensive but less comfortable.
Home Sleep Test – A Simpler device you use at home. More comfortable but less detailed.
The American Academy of Sleep Medicine recommends that both doctors help set your exact pressure settings. Too low won’t help. Too high feels uncomfortable.
Options for Obtaining CPAP Without a Sleep Study
Good news: You don’t always need that uncomfortable overnight lab stay. Several legitimate paths can get you CPAP therapy faster and with less hassle. Here are your real options.
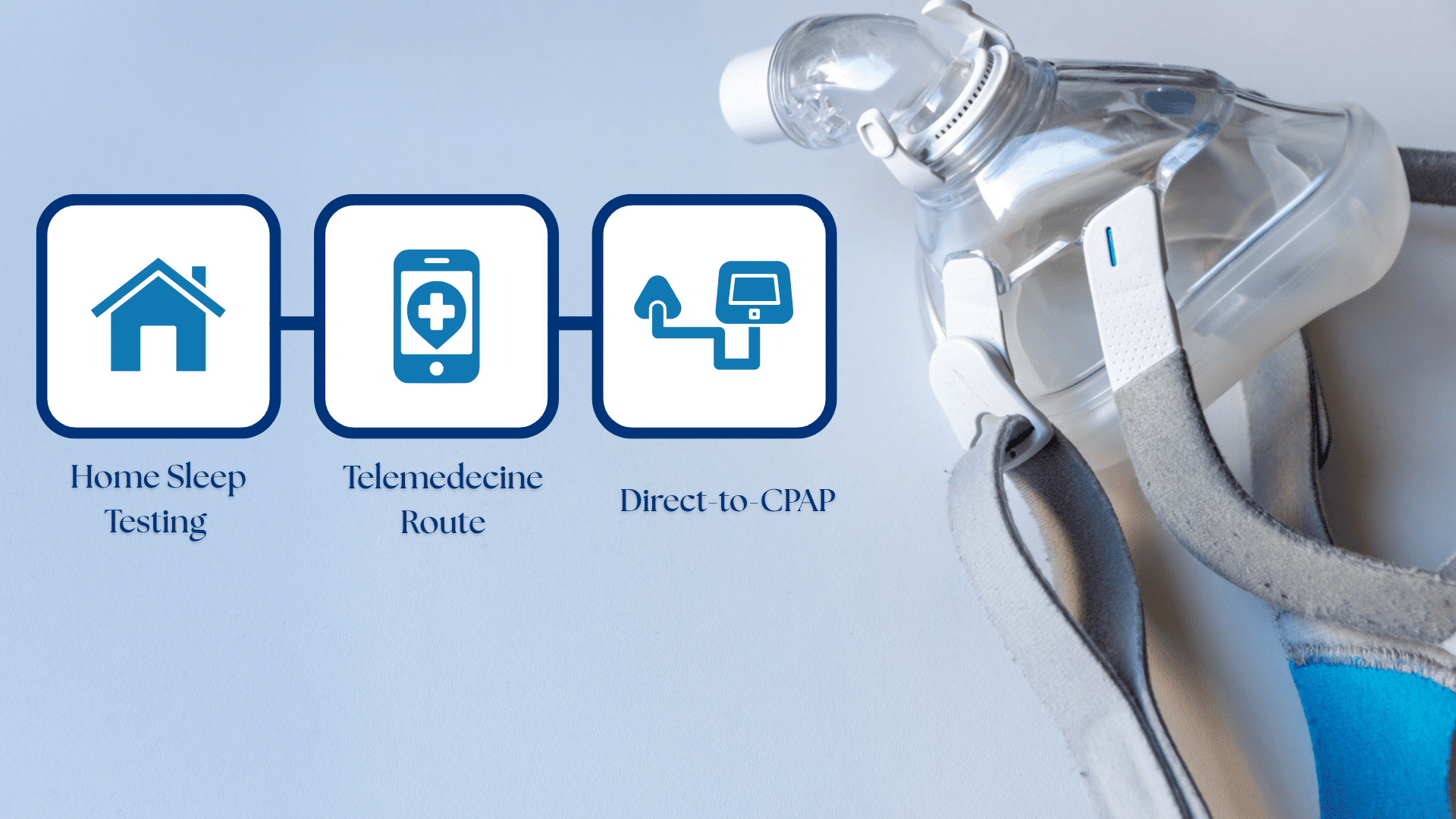
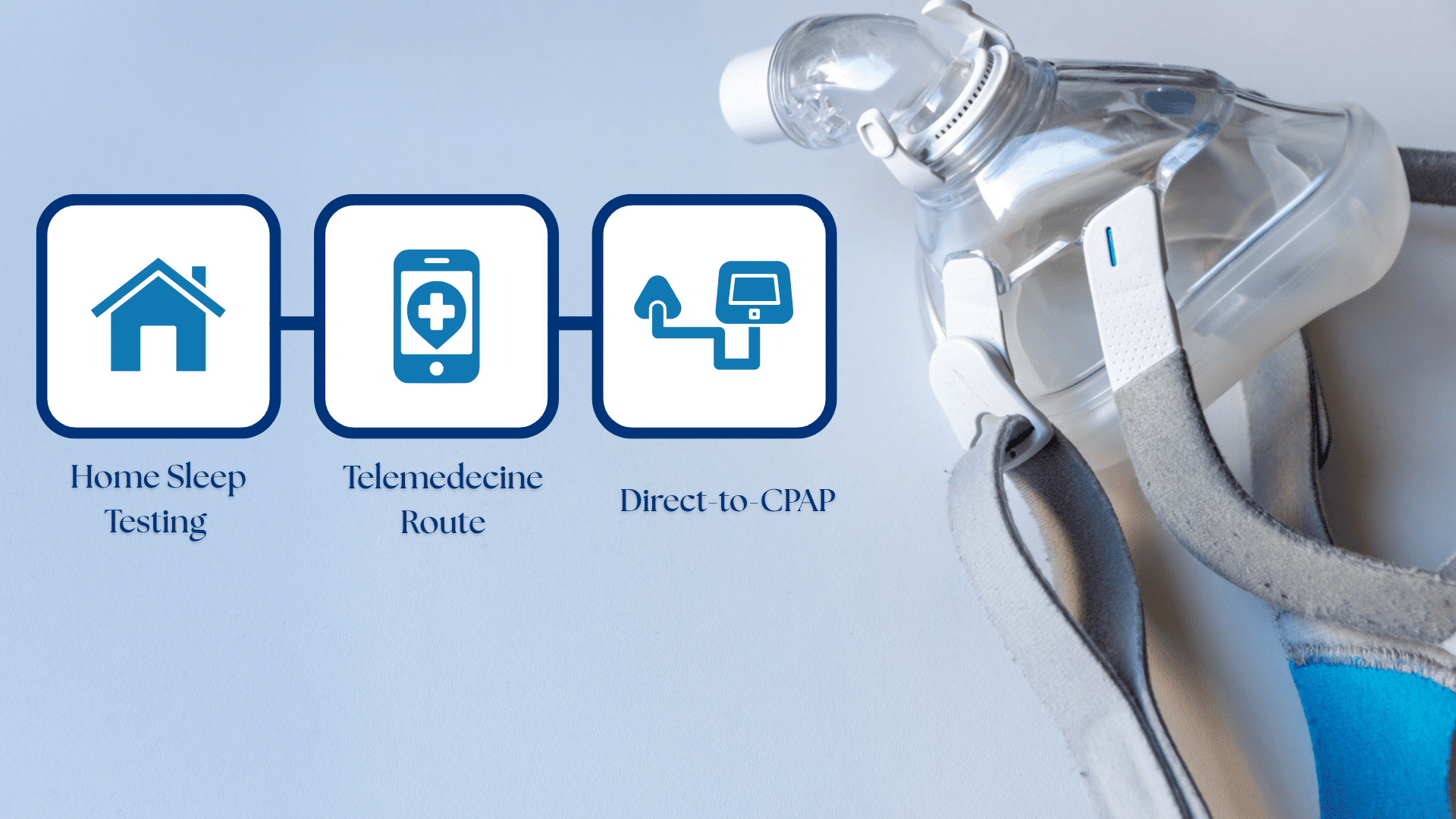
1. Home Sleep Testing (HSAT) & Telemedicine Route
Skip the sleep lab. Test at home instead.
Home Sleep Apnea Tests let you sleep in your own bed. You get a small device that tracks breathing and oxygen levels for 1-3 nights. Return it for analysis. Get results within days.
Studies show home tests are 84% as accurate as lab studies for moderate to severe sleep apnea.
Telemedicine makes it even easier. Fill out an online questionnaire. A doctor reviews your symptoms remotely. If you qualify, they mail you a test kit.
Popular options include Lofta, SleepTest.com, and ApneaMed. The whole process takes 1-2 weeks versus months for traditional testing.
2. Direct-to-CPAP Prescriptions: When It’s Possible
Sometimes doctors skip testing altogether.
This happens with obvious severe symptoms like loud snoring plus witnessed breathing pauses, extreme daytime sleepiness, morning headaches, or high blood pressure despite medication.
Research shows experienced doctors can identify severe sleep apnea based on symptoms alone with 80% accuracy.
Some physicians prescribe CPAP for a trial period. If it helps, you can continue. If not, formal testing follows.
3. Over-the-Counter or Online CPAP Purchase: Is It Legal?
Short answer: No.
The FDA and AASM classifies CPAP machines as Class II medical devices requiring prescriptions.
Wrong pressure settings can be dangerous. Masks need proper fitting. Insurance won’t cover non-prescription devices.
Online “CPAP-like” devices are usually not FDA-approved, less effective, and potentially unsafe. Stick with legitimate routes for your safety.
When Might It Make Sense to Try CPAP Without a Study?
Sometimes the shortcut makes sense. Other times, it’s risky. Here’s how to tell the difference.
You’re Probably Safe to Skip Testing If:
- The partner complains about loud snoring every night
- You wake up gasping or choking
- Fall asleep during meetings or while driving
- Morning headaches won’t go away
- Feel exhausted despite sleeping 8+ hours
- High blood pressure that medicine can’t fix
When Distance is a Problem
Live 200+ miles from a sleep center? Work offshore? Travel constantly for business?
Traditional testing becomes nearly impossible. Home testing makes way more sense than waiting forever. Military deployment and remote jobs also count. Don’t wreck your health waiting months for testing.
When You Should See a Doctor First
Don’t skip testing if you have:
- Heart problems
- Previous stroke
- Lung disease like COPD
- Memory problems or confusion
- You’re under 30 with bad symptoms
- Breathing stops, but no snoring
If other treatments haven’t helped at all, something else might be wrong. See a specialist instead of guessing.
Pros and Cons of Skipping a Formal Sleep Study
Let’s be honest about the trade-offs. Skipping that fancy sleep lab has real benefits. But it also comes with some risks you should know about.
Potential Advantages
Speed is the biggest win. Instead of waiting 3-6 months for a lab appointment, you could have a CPAP machine within weeks. That’s months of better sleep you’re not missing out on.
Your wallet will thank you, too. Home sleep tests cost $150-$500 compared to $1,000-$3,000 for lab studies. Even with insurance, your out-of-pocket costs drop significantly.
No lab anxiety. Some people just can’t sleep with strangers watching them. The wires, the unfamiliar bed, the clinical setting – it all feels weird. Home testing eliminates that stress completely.
The convenience factor is huge. Sleep in your own bed. Use your own pillow. Follow your normal routine. The results are often more accurate because you’re actually sleeping normally.
Risks & Dangers of Bypassing Diagnosis
Here’s where things get tricky. Skipping proper diagnosis isn’t always harmless.
| Risk | Potential Problem |
|---|---|
| Wrong Pressure Settings | Still stop breathing or uncomfortable air pressure |
| Missing Other Sleep Disorders | Restless leg, narcolepsy need different treatments |
| No Medical Oversight | Problems and side effects go unnoticed |
| Insurance Issues | Claims denied, coverage gaps |
| Worsening Symptoms | Poor treatment is sometimes worse than none |
Bottom line: These risks are real but manageable. Most people with obvious sleep apnea symptoms do fine with alternative routes. But if you have complex medical conditions or unusual symptoms, the full lab study might be worth the hassle.
Medical & Legal Considerations Before You Proceed
Before you jump into any CPAP shortcut, understand what you’re getting into. Some risks are worth taking. Others aren’t.
Health Risks of Improper CPAP Use
Using CPAP wrong can backfire badly.
Too much air pressure can over-inflate your lungs, causing chest pain or a collapsed lung. This happens in 0.5% of users with incorrect settings.
CPAP might mask serious underlying problems like heart conditions or neurological disorders that need different treatments entirely.
Wrong settings can also disrupt your natural breathing patterns, making you dependent on the machine.
Insurance Coverage and Prescription Requirements
Reality check: Most insurance requires documented sleep studies for CPAP coverage. No exceptions.
Without proper documentation, expect $800-$3,000 out-of-pocket for the machine. Monthly supplies add $50-$100 more.
Even alternative routes often require compliance data within 90 days. Fail to meet requirements? Insurers can demand full repayment.
Check with your insurance first. The “shortcut” might cost more than the traditional route.
Alternatives to Using CPAP Without Diagnosis
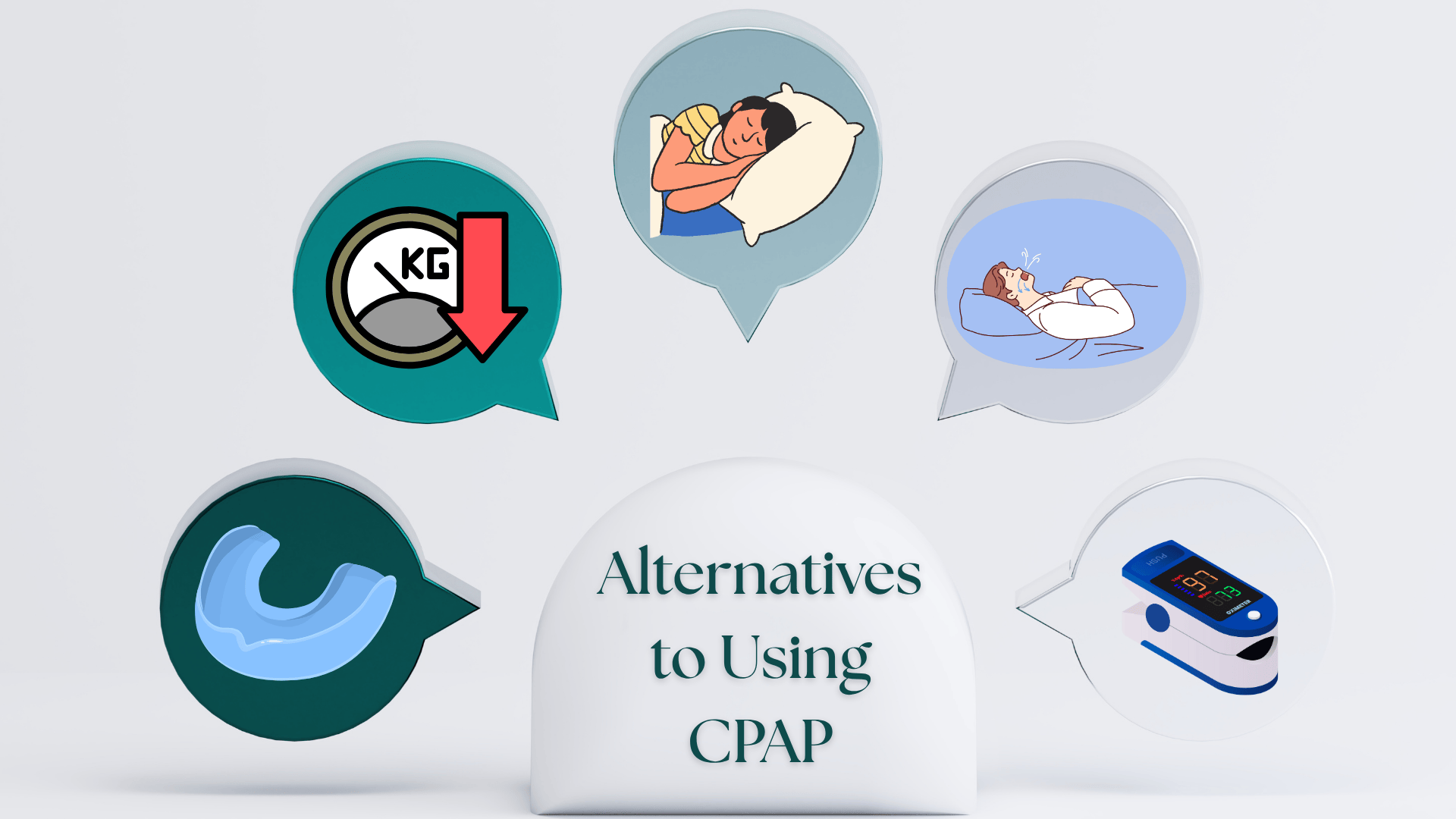
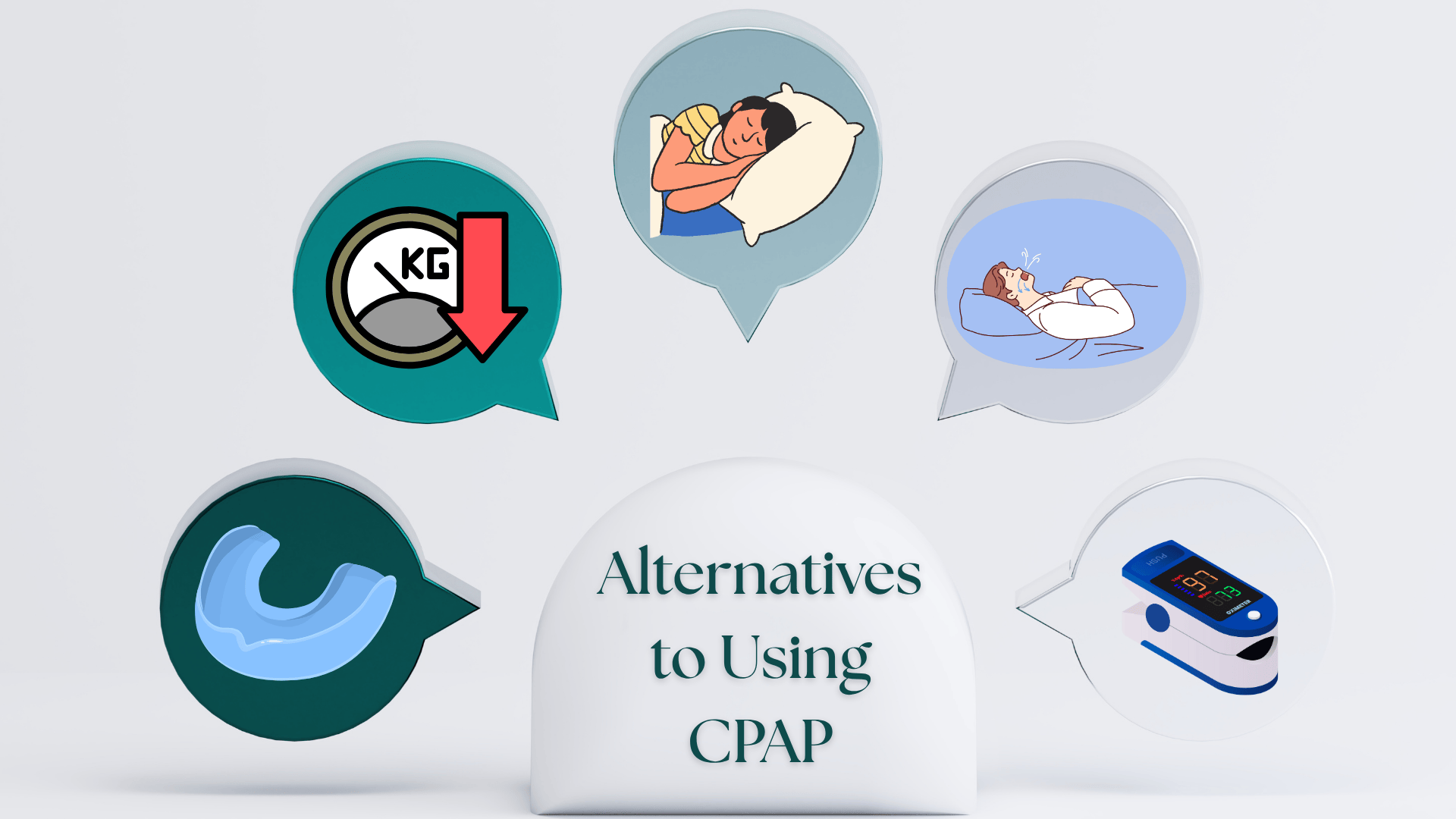
Not ready to commit to CPAP? Smart move. Try these options first while you figure out your long-term plan.
Non-CPAP Treatments Until You’re Evaluated
- Oral Appliances: Custom mouthpieces push your jaw forward, keeping airways open. 70% as effective as CPAP for mild cases. No machine needed.
- Positional Therapy: Sleep on your side instead of your back. A tennis ball in a pajama shirt works. Modern vibrating devices nudge you to roll over.
- Weight Loss: Losing 10% of body weight reduces apnea episodes by 26%. Takes time, but most sustainable solution.
- Upper Airway Stimulation: An implanted device stimulates the tongue muscle. FDA-approved but requires surgery and costs $30,000+.
Lifestyle Measures & Self-Monitoring
Sleep Tracking:
- Keep a sleep log (bedtime, wake time, morning energy)
- Use the Epworth Sleepiness Scale (2-minute questionnaire)
- Try the STOP-Bang screening tool
Home Monitoring:
- Pulse oximeter shows overnight oxygen drops ($20-$50)
- Phone apps like SnoreLab record snoring patterns
- Partner logs witnessed breathing pauses
This data helps doctors make faster, more accurate treatment decisions.
Getting the Sleep You Deserve
Your sleep matters. Your health matters. And you don’t have to suffer through months of waiting just to breathe properly at night.
Just be smart about it. If you have obvious symptoms and no serious medical conditions, alternative routes make sense. If you have heart problems or unusual symptoms, see a specialist first.
The worst choice? Doing nothing while your health gets worse.
What’s your experience been like? Drop a comment below and let us know which route you took to get CPAP therapy. Your story might help someone else who’s struggling with the same decision.